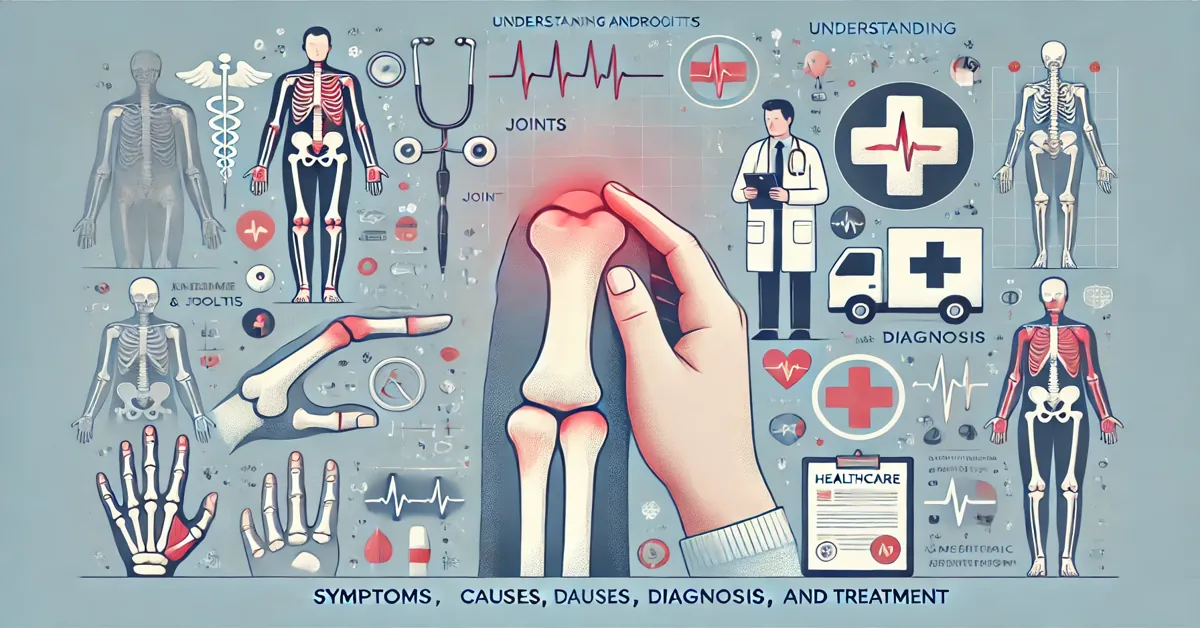
Andrigolitis is an inflammatory joint condition that affects both men and women, though it is more commonly seen in men. The term itself is derived from the Greek words “andros” meaning man, and “itis,” which refers to inflammation. This condition specifically targets the joints, leading to pain, swelling, and stiffness. While andrigolitis is less well-known compared to other joint-related disorders such as arthritis or tendinitis, it still poses significant challenges to those affected.
Despite its less publicized presence in the medical world, andrigolitis shares many similarities with other inflammatory conditions, and its symptoms can sometimes overlap with those of more recognized joint diseases. This article aims to provide an in-depth understanding of andri golitis, exploring its symptoms, causes, diagnostic procedures, treatment options, and preventive measures.
What is Andrigolitis?
Andrigolitis is primarily characterized by inflammation in the joints, leading to discomfort and a reduction in mobility. Unlike arthritis, which can result from autoimmune disorders or simple wear and tear, andri golitis tends to target the joints in a manner that suggests inflammation is the primary driver of pain and stiffness. While the condition is often associated with men, it can also impact women, particularly those with certain genetic predispositions.
Though andrigolitis can affect any joint, it most commonly impacts larger joints such as the knees, hips, and shoulders, as well as smaller joints like those found in the fingers. Like many other joint disorders, andri golitis can significantly impair day-to-day activities, especially if left untreated.
Symptoms of Andrigolitis
Recognizing the symptoms of andrigolitis is crucial for early diagnosis and effective management. The symptoms can be similar to other joint inflammation disorders, making it easy to confuse andri golitis with conditions like arthritis or tendinitis. However, certain distinctive features of andri golitis can help differentiate it from other joint issues.
Here are the most common symptoms associated with andrigolitis:
- Pain in the Joints: The primary symptom of andri golitis is joint pain, which often worsens with movement or activity. The pain can range from mild to severe and may fluctuate in intensity over time.
- Swelling: Inflammation typically leads to swelling around the affected joints, which can cause stiffness and discomfort. The skin around the joints may also appear red and feel warm to the touch.
- Stiffness: Morning stiffness or difficulty moving the joints after periods of inactivity is a hallmark symptom of andri golitis. The stiffness often improves with movement but can return after long periods of rest.
- Reduced Range of Motion: Over time, andri golitis can limit the range of motion in affected joints, making it challenging to perform regular activities like bending, reaching, or walking.
- Joint Tenderness: The affected joints may feel tender when touched, especially during flare-ups of inflammation.
- Weakness: Muscle weakness around the affected joint may develop, particularly if the pain and inflammation discourage regular use of the joint.
These symptoms can occur in a single joint or multiple joints, and their intensity can vary based on factors like activity level, overall health, and the presence of underlying conditions.
Causes and Risk Factors of Andrigolitis
Understanding the causes and risk factors of andrigolitis is essential for both prevention and treatment. Although the exact cause of andri golitis remains elusive, several contributing factors have been identified:
1. Inflammatory Response
Like other inflammatory joint conditions, andrigolitis may stem from an overactive inflammatory response in the body. Inflammation is a natural immune response, but when it becomes chronic or excessive, it can lead to joint damage and pain. In andri golitis, this inflammation primarily targets the joints, causing swelling and discomfort.
2. Genetic Predisposition
Genetics appear to play a role in the development of andrigolitis. Individuals with a family history of inflammatory joint diseases, such as arthritis or ankylosing spondylitis, may be at a higher risk of developing andri golitis. Certain genes involved in regulating the immune system may contribute to the overactive inflammatory response seen in this condition.
3. Gender
While andrigolitis can affect both men and women, it is more commonly seen in men, particularly in middle age. The reasons for this gender disparity are not fully understood, but it may relate to hormonal differences or genetic factors that predispose men to inflammatory joint conditions.
4. Injury or Trauma
Previous joint injuries or trauma can increase the risk of developing andrigolitis. Damaged joints are more vulnerable to inflammation, which can trigger the onset of andri golitis in susceptible individuals.
5. Occupational Hazards
People who engage in repetitive physical activities or heavy labor are at an increased risk of joint injuries, which can lead to chronic inflammation and the development of andrigolitis. Jobs that require repetitive movements, lifting heavy objects, or extended periods of standing can put strain on the joints, increasing the likelihood of inflammation.
6. Age
As with many inflammatory conditions, the risk of developing andri golitis increases with age. Older adults are more likely to experience joint wear and tear, which can exacerbate inflammation and lead to the onset of andrigolitis.
7. Autoimmune Disorders
Although not as commonly linked to andrigolitis as with other joint conditions, autoimmune disorders that trigger an overactive immune response can sometimes play a role in the development of the condition. People with autoimmune disorders are more prone to chronic inflammation, which can affect the joints and lead to andrigolitis.
Diagnosis of Andrigolitis
Diagnosing andrigolitis can be challenging due to the similarity of its symptoms to other joint disorders. However, a thorough evaluation by a healthcare professional can help differentiate andrigolitis from other conditions like arthritis or tendinitis. The diagnostic process typically involves several steps:
1. Medical History
Your doctor will begin by taking a detailed medical history, including questions about your symptoms, family history of joint disorders, and any previous injuries or traumas. Understanding your personal and family medical history is crucial for identifying potential risk factors for andrigolitis.
2. Physical Examination
A physical examination will follow, during which the doctor will assess the affected joints for signs of swelling, tenderness, redness, and warmth. The doctor may also test your range of motion to determine if joint stiffness or weakness is present.
3. Imaging Tests
Imaging tests like X-rays, MRIs, or CT scans are often used to assess the condition of the joints. These tests can help identify joint damage, inflammation, or any structural abnormalities that may be contributing to your symptoms.
4. Blood Tests
Blood tests may be ordered to check for markers of inflammation, such as elevated levels of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR). These tests can provide insight into the level of inflammation in your body and help rule out other inflammatory conditions like rheumatoid arthritis.
5. Joint Fluid Analysis
In some cases, a joint fluid analysis may be performed. This involves drawing a small amount of fluid from the affected joint to test for signs of infection, inflammation, or other abnormalities. This test can help confirm a diagnosis of andrigolitis and rule out other causes of joint pain.
Treatment Options for Andrigolitis
Once diagnosed with andrigolitis, your healthcare provider will develop a personalized treatment plan to manage your symptoms and reduce inflammation. Treatment for andrigolitis typically involves a combination of medications, lifestyle changes, and physical therapy.
1. Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to reduce inflammation and relieve pain. These medications can help manage the symptoms of andrigolitis, making it easier to perform daily activities.
- Corticosteroids: For more severe cases of andrigolitis, corticosteroids may be prescribed to quickly reduce inflammation. These medications can be taken orally or injected directly into the affected joint for fast relief.
- Disease-Modifying Antirheumatic Drugs (DMARDs): In cases where andrigolitis is linked to an autoimmune response, DMARDs may be prescribed to suppress the immune system and prevent further joint damage.
2. Physical Therapy
Physical therapy is often recommended for people with andrigolitis to help improve joint mobility and strengthen the muscles around the affected joints. A physical therapist can develop an exercise program tailored to your needs, which may include stretching, strengthening, and range-of-motion exercises.
3. Lifestyle Modifications
Making certain lifestyle changes can help reduce the frequency and severity of andrigolitis flare-ups. These may include:
- Weight Management: Maintaining a healthy weight can reduce the strain on your joints, lowering the risk of inflammation.
- Exercise: Regular low-impact exercise, such as swimming or cycling, can help improve joint flexibility and reduce stiffness.
- Rest: It’s important to balance activity with rest, especially during periods of flare-ups when your joints need time to recover.
4. Surgery
In severe cases of andrigolitis, when conservative treatments fail to provide relief, surgery may be considered. Surgical options include joint repair, joint replacement, or joint fusion, depending on the extent of the damage and the specific joint involved.
Preventing Andrigolitis
While it may not always be possible to prevent andrigolitis, there are steps you can take to reduce your risk and protect your joints:
- Avoid Joint Injuries: Take precautions to avoid joint injuries, such as wearing appropriate protective gear during sports and using proper techniques when lifting heavy objects.
- Maintain a Healthy Weight: Keeping your weight within a healthy range can reduce the strain on your joints, lowering your risk of inflammation.
- Stay Active: Regular exercise can help keep your joints flexible and reduce the risk of stiffness and inflammation.
- Eat a Balanced Diet: A diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can help reduce the risk of chronic inflammation.
Conclusion
Andrigolitis may not be as widely known as other inflammatory joint conditions, but it poses significant challenges for those who suffer from it. By understanding the symptoms, causes, diagnosis, and treatment options for andrigolitis, individuals can take proactive steps to manage the condition and improve their quality of life. Whether through medications, physical therapy, lifestyle changes, or preventive measures, there are many ways to reduce the impact of andrigolitis and maintain healthy, pain-free joints.